What is keratoconus?
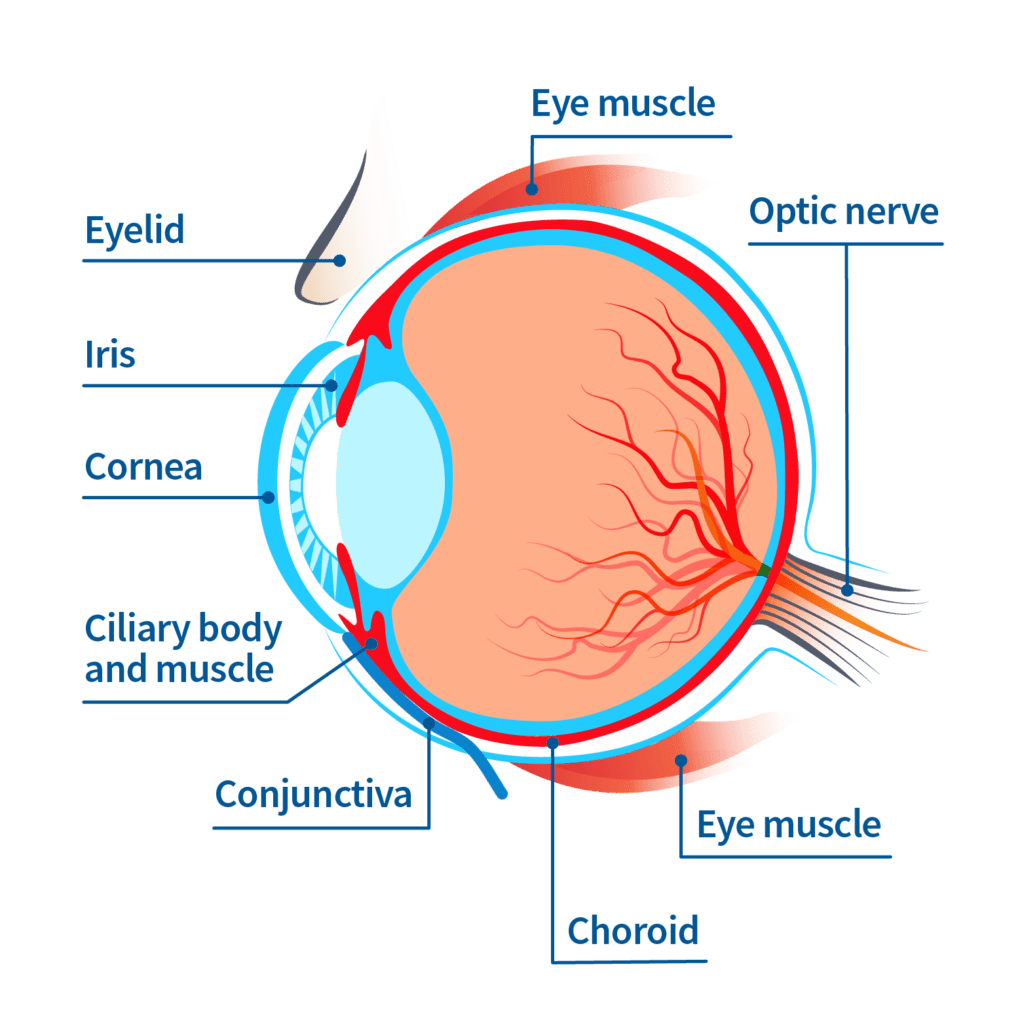
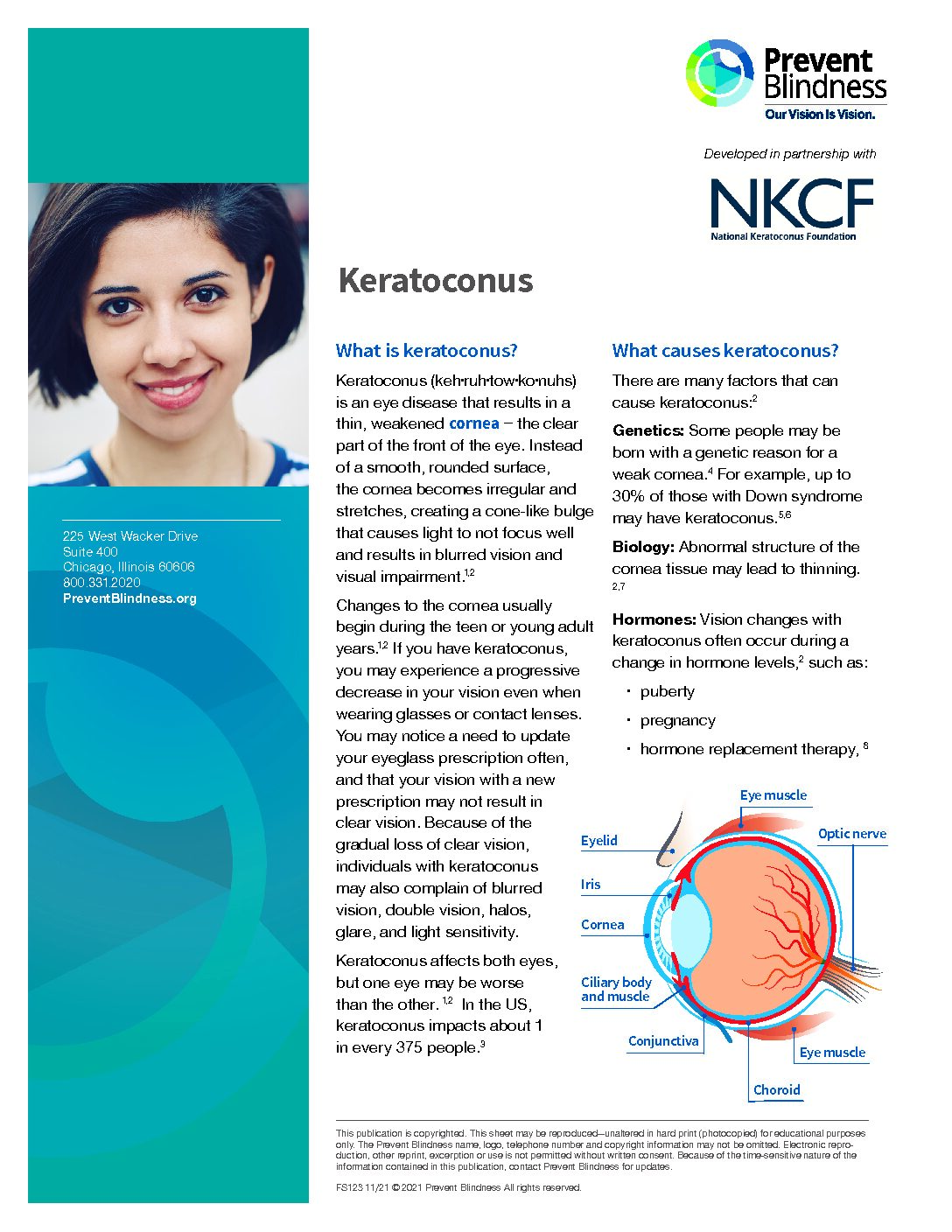
Keratoconus (keh·ruh·tow·ko·nuhs) is an eye disease that results in a thin, weakened cornea – the clear part of the front of the eye. Instead of a smooth, rounded surface, the cornea becomes irregular and stretches, creating a cone-like bulge that causes light to not focus well and results in blurred vision and visual impairment.
Changes to the cornea usually begin during the teen or young adult years. If you have keratoconus, you may experience a progressive decrease in your vision even when wearing glasses or contact lenses. You may notice a need to update your eyeglass prescription often, and that your vision with a new prescription may not result in clear vision. Because of the gradual loss of clear vision, individuals with keratoconus may also complain of blurred vision, double vision, halos, glare, and light sensitivity. Keratoconus affects both eyes, but one eye may be worse than the other. In the US, keratoconus impacts about 1 in every 375 people.

normal cornea

keratoconic cornea
What causes keratoconus?
There are many factors that can cause keratoconus:
Genetics: Some people may be born with a genetic reason for a weak cornea. For example, up to 30% of those with Down syndrome may have keratoconus.
Biology: Abnormal structure of the cornea tissue may lead to thinning. 2,7 Hormones: Vision changes with keratoconus often occur during a change in hormone levels, such as:
- puberty
- pregnancy
- hormone replacement therapy
Allergies and eye rubbing: Many people with keratoconus also suffer from allergies or other irritations of the eyes, which causes them to rub their eyes. Forceful eye rubbing may result in small traumas to already weak corneas.9 Managing your allergies and other irritants to prevent eye rubbing can be an important step in controlling keratoconus. Other associated diseases include atopic diseases, and connective tissue or collagen disorders such as floppy eyelid syndrome, obstructive sleep apnea, mitral valve prolapse and Ehlers-Danlos syndrome.
Family history: Close relatives of individuals with keratoconus (such as parents and siblings) are at higher risk for the disease.
Certain environments: Keratoconus occurs in all countries, but climates that are sunny, dry and dusty seem to have a higher rate of keratoconus – likely because the environments can cause more eye irritation.
Ethnicity: Certain ethnic groups are at higher risk – from certain countries such India, Pakistan, Iran, Saudi Arabia, and Polynesia.
How is keratoconus diagnosed?
Vision changes (blurred vision) due to myopia (nearsightedness) are usually noticed during the teen years. Nearsightedness can be easily corrected with glasses or contact lenses and usually results in 20/20 or better vision. Keratoconus can also cause blurred vision, but because of the irregular cornea, glasses and contact lenses do not correct the vision to 20/20. In fact, if a teen with blurred vision cannot be corrected to 20/20, one of the most common causes is keratoconus. Any teen that cannot see 20/20 with glasses should be evaluated for some other eye problem.
An eyecare provider will conduct a thorough examination to diagnose keratoconus. The examination will include the following:
Medical history: Personal and family medical history
Topography or tomography: The doctor may also use special imaging such as topography or tomography to create a detailed map of the height and shape of the cornea. This test will also measure the thickness of the cornea.
Keratometry: Keratometry focuses a circle of light on the cornea and measures the reflection to determine the shape (normal or abnormal) of the cornea.
Genetic testing: Genetic factors interact with environmental factors to cause keratoconus. Genetic eye testing is now available to screen for variants that can cause keratoconus. This testing will help to identify those at high-risk to allow for earlier intervention and treatment.
How is keratoconus treated?
Currently, there is no cure for keratoconus, but there are several effective treatments.
Contact lenses: When prescription eyeglasses no longer provide adequate vision correction, scleral lenses or rigid gas permeable (GP) lenses can correct irregular corneas by providing a smooth ocular surface.21 If you have mild keratoconus, which does not progress (get worse over time), contact lenses may be the best and only treatment needed.
Corneal crosslinking (CXL): If your eye doctor documents progression of your keratoconus using the high-resolution imaging devices, they may recommend corneal CXL. CXL is a one-hour treatment that combines riboflavin (Vitamin B) eyedrops and ultraviolet light to halt the progression of keratoconus.22 This treatment reduces the stretching and thinning of the cornea that is associated with worsening of the disease and vision loss. The procedure is well-tolerated, has a high success rate, and contact lenses can still be worn following the procedure. This procedure can have some side effects, but fortunately these are rare. If you are interested in this treatment, ask your corneal surgeon to see if it is right for you.

Rigid gas permeable (GP) contact lenses are hard or rigid contact lenses are smaller than scleral lenses and rest only on the cornea. Scleral lenses are large rigid gas permeable contact lenses that rest on the white part of the eye (sclera) and arch over the cornea. They are bigger than rigid gas permeable lenses.
Corneal transplant: If the keratoconus progresses to the point where your vision is severely affected, contact lenses are no longer helpful and/or are painful to wear, or if scars form on the cornea, then a corneal transplant may be recommended. A corneal transplant is when a diseased cornea is replaced with a clear healthy cornea from a human donor. In general, corneal transplants for keratoconus are considered to be the most successful of all corneal transplants and result in improved vision in most patients (though often eyeglasses or contact lenses are still needed). However, currently this surgical treatment is reserved for the most severe cases.
With the introduction of more advanced diagnostic tools, improved contact lens technology and corneal crosslinking therapy, keratoconus has become an eye disease that can be managed very effectively.