What is Stargardt disease?
Stargardt disease, also called Stargardt macular dystrophy, causes vision loss due to a buildup of fatty material in the macula. The macula is a small area in the center of the retina that is responsible for sharp, straight-ahead vision. Stargardt disease is a rare eye genetic disease – part of a group of conditions called inherited retinal diseases (or IRDs), generally caused by a variation in one or more genes, causing the gene to not work properly. Stargardt disease affects about 1 in 10,000 people in the United States.
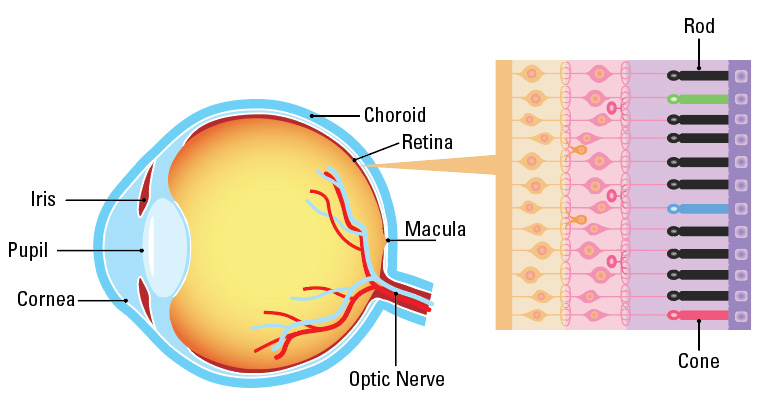 A diagram of the eye
A diagram of the eye
Stargardt Fact Sheets to Print and Share
Stargardt disease typically causes central vision loss in both eyes during childhood or adolescence, but sometimes it occurs later in life. Central vision loss can cause difficulty recognizing faces and reading. Side (peripheral) vision is usually not affected, so it is rare for a person with Stargardt disease to lose all of their vision.
The rate of vision loss is different for each person. For some, Stargardt disease starts out slowly, then speeds up and levels off. At about 20/40 vision (meaning someone sees at 20 what a person with typical vision sees at 40 feet), vision loss can speed up. Vision may rapidly get worse until it reaches about 20/200.
After this point, vision usually stays about the same and cannot be corrected with eyeglasses, contact lenses or refractive surgery.
Focus on Eye Health Expert Series:
Stargardt Disease
In this episode of the Focus on Eye Health Expert Series, Prevent Blindness president and CEO, Jeff Todd, discusses Stargardt disease, genetic testing, clinical trials, and mental health concerns with Elias Traboulsi, MD, MEd, Pediatric Ophthalmologist and Geneticist, Department of Ophthalmology, Cleveland Clinic.
Dr. Traboulsi is not affiliated with the sponsor of this video, nor has he received financial compensation for participating in the interview.
Learn more about eye and vision health
by subscribing to the Prevent Blindness YouTube channel
What causes Stargardt disease?
Stargardt disease is most commonly caused by a variant in the ABCA4 gene. The variant gene is what causes the build-up of extra fatty material in the retina.
Normally, when the retina processes light, there is leftover fatty material that gets taken away by different parts of the eye. With Stargardt disease, the fatty material builds up and damages the photoreceptors. Photoreceptors (rods and cones) are a special part of the retina used to process light and help us see. When our photoreceptors don’t work well, there can be problems with vision.
The mutated ABCA4 gene must be passed down from both parents in order for it to cause eye problems. If only one parent has the mutated ABCA4 gene, then their child will be a carrier of the disease but won’t have the disease themselves, and their vision will not be affected. Both parents must pass on the variant ABCA4 gene in order for the child to have vision loss due to Stargardt disease.
There are a few other genes in which a mutation can cause retinal disease that looks similar to Stargardt disease on eye examination and have similar symptoms. These genes include PRPH2, ELOVL4, and PROM1. Mutations in these genes are inherited differently. Depending on which gene is responsible for a person’s eye condition, it may have different effects on disease severity and different risk to other family members.
What are Genes?
Cells are the basic building blocks of all living things.
The command center of each cell is called the nucleus, and it contains chromosomes.
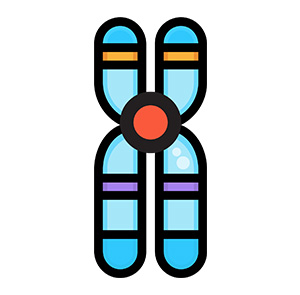
Chromosomes are made up of DNA—the body’s hereditary material.
A gene is a small section of DNA that contains the instructions for a specific molecule in the body, which is passed from parent to child.
Each gene contains the information required to build specific proteins needed in the body, for example, proteins build bones, determine eye color, allow muscles to move, control digestion, and keep your heart beating.
If there is a change in a gene’s DNA sequence, it is called a variant. Not all variants cause disease. A disease-causing variant is called a mutation.
What are symptoms of Stargardt disease?

How a person with Stargardt disease sees
The most common symptom of Stargardt disease is a slow loss of central vision in both eyes. Some people lose their central vision more quickly than others. Rarely, a small number of people with Stargardt disease may also lose their side (peripheral) vision. It is unusual for someone to lose all vision due to Stargardt disease.
The age when blurry vision starts can predict how much vision will change as they age. For example, an individual with Stargardt disease who has blurry vision earlier in life will usually have worse vision than someone with Stargardt disease whose vision becomes blurry when they are older.
Other symptoms may include:
- Dark, gray, black, or hazy spots in the center of your vision
- Sensitivity to light
- Blurry vision that cannot be corrected with glasses
- Difficulty seeing small details
- Needing more time for your eyes to adjust between light and dark places
- Difficulty seeing in the dark or low light
- Color blindness
- Lack of depth perception
- Lack of contrast
You may not experience all the symptoms from the list above. Symptoms for each person will vary depending on your age, stage of the disease, and genetic variation.
How is Stargardt disease diagnosed?
Diagnosis of Stargardt disease may take longer than other, more commonly occurring vision conditions. The diagnosis typically starts during an eye examination with an eye doctor. If the eye doctor thinks that you have an IRD, such as Stargardt disease, they will ask you to see a retina specialist or an eye doctor more experienced in diagnosing and treating IRDs. The retina specialist will conduct further testing to confirm your diagnosis. They will conduct a very detailed examination including the steps listed below.
The goals of the detailed examination are to:
- Establish the specific diagnosis.
- Get the treatment that is right for that diagnosis.
- Connect the patient to supportive services such as a genetic counselor (someone that specializes in the genetic testing process and educating patients) and vision rehabilitation.
- Educate other family members about their risk for the disease.
- Provide information to the patient about clinical trials and new therapies.
Initial and follow-up examinations
These examinations may include the following:
Patient history: Including current vision issues, patient medical history, current medications, and past medication use.
Family history: Constructing a family medical history to show the genetic relationships and medical disorders that occur in a family. From the family medical history, patterns of familial disorders and how diseases were passed down may emerge. This leads doctors to a clear diagnosis of the genetic disorder and allows assessments for family members who may also be at risk for the disorder.
Clinical eye examination
The eye examination includes:
Dilation: Eye drops are put into the eye to widen the opening on the front of the eye, called the pupil. This allows the eye doctor to examine the health of the retina.
Visual Acuity: A measure of the ability to see detail up close and in the distance.
Color vision testing: Stargardt disease can cause color blindness, so your eye doctor may also test your color vision.
Slit lamp: A non-invasive procedure that uses a microscope and bright light to look at different parts of the eye.
Indirect ophthalmoscopy: A noninvasive tool worn by the eye doctor that provides magnification, allowing them to examine the back of the eye.
Imaging: The eye doctor will conduct a series of imaging tests to view different parts of the eye, including:
- Retinal photographs: A photo taken of the inside surface of the eye.
- Optical Coherence Tomography (OCT): A test that takes crosssectional pictures of the retina. This allows your ophthalmologist to map and measure the thickness of the retina.
- Fundus autofluorescence: A test used to create a density map of the layers of the retina.
- Infrared autofluorescence: A test that provides information on the distribution of pigment in the retina.
- Fluorescein angiography: A test that uses a fluorescent dye injected in the vein of the arm or hand and pictures taken of the retina through dilated pupils.
Visual Field Testing: A test that measures central and side or peripheral vision.
Electroretinography (ERG): A test to measure the electrical response of the eye’s light-sensitive cells, called rods and cones. During the test, the eye doctor will place drops into your eyes, so you will not have any discomfort during the test.
Genetic testing: Patients may meet with a genetic counselor (someone that specializes in the genetic testing process and educating patients) to determine the testing approach that is best based on the other test results. Patients are often asked to provide a blood or saliva sample that will be sent to a lab for analysis. The genetic test confirms or disputes the diagnosis of a specific IRD, so that correct information is provided to the patient and family. Genetic testing is often a requirement for participation in IRD-related clinical research trials.
Why is Genetic Testing Important?
Identifying the genetic cause of disease is an important part of care for patients with Inherited Retinal Diseases (IRDs). Many times, the exact type of IRD a person has can be difficult to determine based only on tests conducted in the eye doctor’s office. Results from genetic testing can lead to an accurate diagnosis if there is a positive finding. Having the genetic diagnosis may help to:
- Identify potential treatment options or clinical trial options for patients.
- Inform them about the potential risk of disease to other family members.
- Identify the potential risk to other organs in the patient’s body that may be affected.
- In the case of infants and young children, genetic testing will identify those children who are at risk of other health problems and who will benefit from early diagnosis and therapy.
- Inform a person about what will happen to their vision over time.
A health care provider will order the genetic test, collect the sample, and review the results with the patient. Ideally, the health care provider would include a genetic counselor to guide the patient and their family through the results of the genetic testing, discuss the impact on other family members, and assist couples who have questions around family planning decisions. It may be helpful to have genetic testing done if you are interested in joining a clinical trial, or if it has been several years since your last genetic test was completed.
Complete genetic testing.
Learn more about IRDs and benefits of genetic testing.
Find a provider to help you access genetic testing.
The Foundation Fighting Blindness’s list of Retina Doctors makes it easy to find a genetic testing specialist or health care provider in your area of the United States who can discuss your testing options and assist you in learning more about your IRD.
What is the treatment for Stargardt disease?
There is currently no FDA-approved treatment for Stargardt disease, however, there are several clinical trials in process that may lead to treatment options. Continue to see your eye doctor every 1-2 years or as recommended. It is important to check your eyes regularly as other eye health conditions can occur.
If at any time you feel there has been a change in your vision, you should see an eye doctor and have a dilated eye examination. It is also important to have a current record of an eye exam if you would like to join a clinical trial.
Questions to ask your doctor
How do I manage living with Stargardt disease?
Can you suggest a vision rehabilitation center in my area?
How often do you recommend getting an eye exam?
Are there foods with vitamin A I should avoid?
Am I eligible to take part in a clinical trial?
Should I speak to a genetic counselor and get genetic testing?
Are there eyeglasses, contact lenses, or a combination of the two that can help me see a little clearer?
Can you suggest things that will help me cope with my vision loss?




