What is glaucoma?
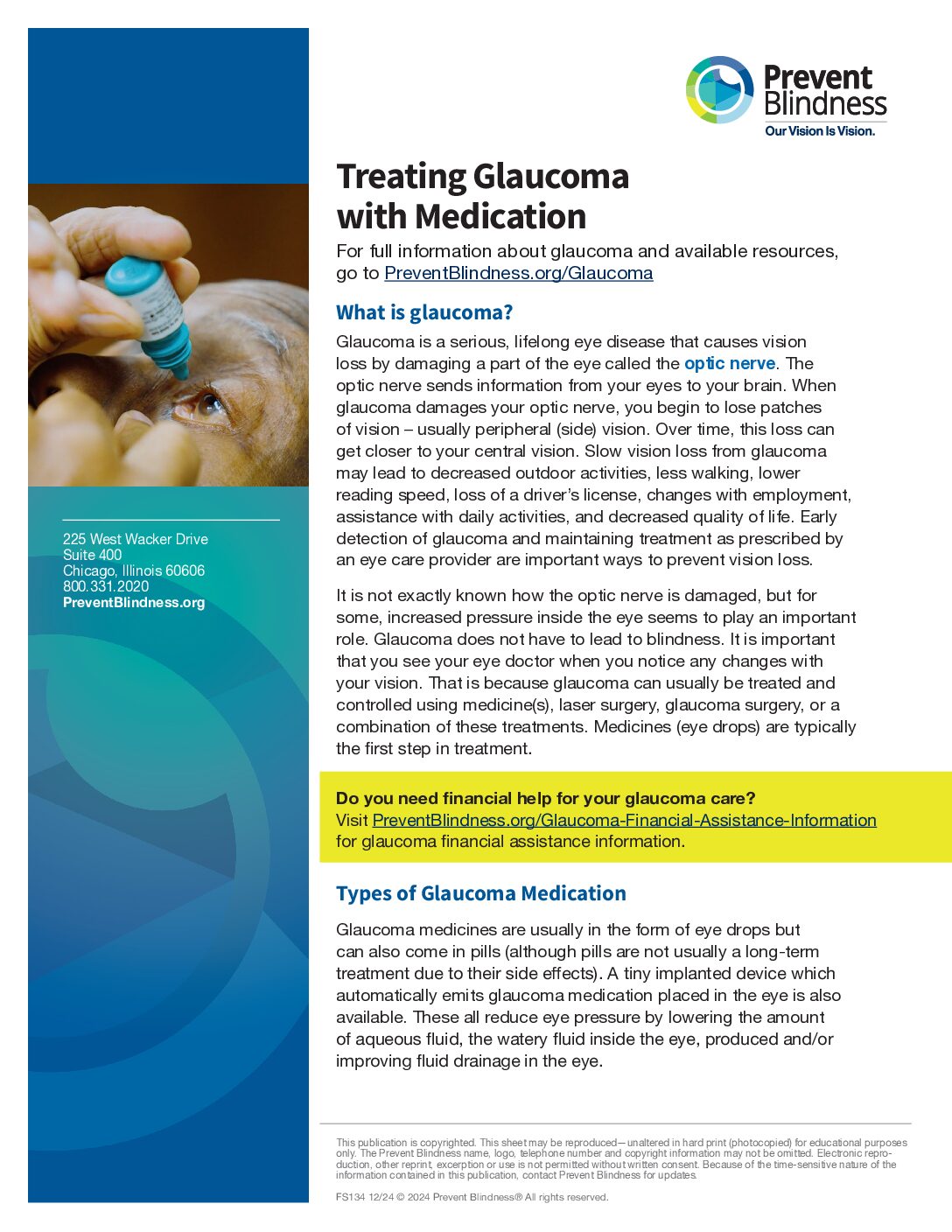
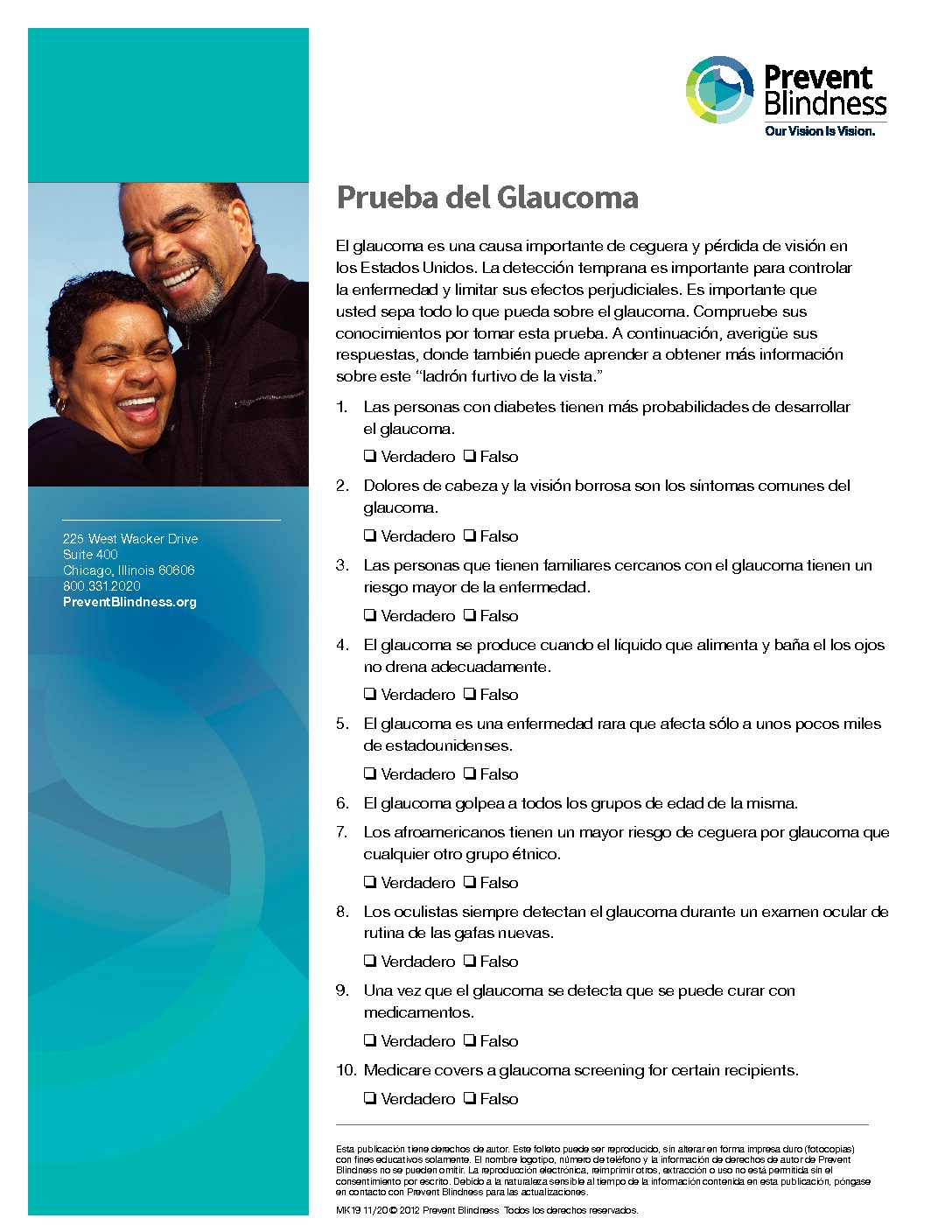
Glaucoma is a serious, lifelong eye disease that causes vision loss by damaging a part of the eye called the optic nerve. The optic nerve sends information from your eyes to your brain. When glaucoma damages your optic nerve, you begin to lose patches of vision – usually peripheral (side) vision.
Over time, this loss can get closer to your central vision. Slow vision loss from glaucoma may lead to decreased outdoor activities, less walking, lower reading speed, loss of a driver’s license, changes with employment, assistance with daily activities, and decreased quality of life. Early detection of glaucoma and maintaining treatment as prescribed by an eye care provider are important ways to prevent vision loss
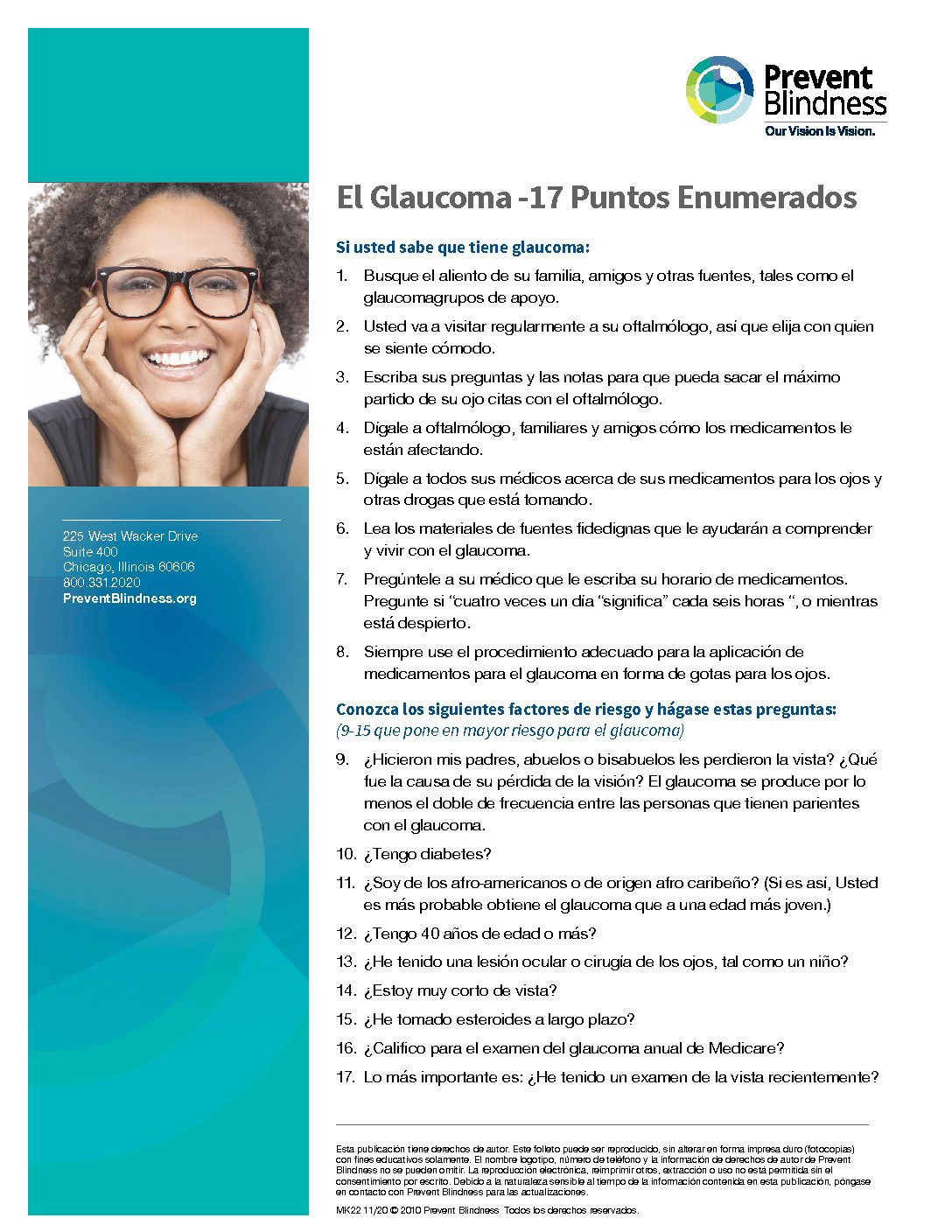
Glaucoma does not have to lead to blindness. It is important that you see your eye doctor when you notice any changes with your vision. That is because glaucoma can usually be treated and controlled using medicine(s), laser surgery, glaucoma surgery, or a combination of these treatments. Medicines (eye drops) are typically the first step in treatment.
How does glaucoma damage my eyes?
Glaucoma causes damage to the optic nerve. Although glaucoma can occur at almost any eye pressure, increased eye pressure seems to play an important role, and lowering the eye’s pressure can decrease further vision loss.
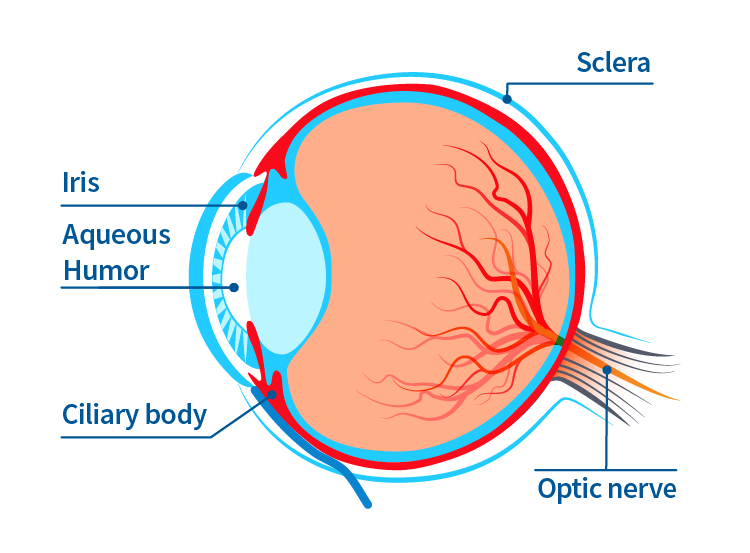
Your eye produces a watery fluid called aqueous humor. When your eye is healthy, the fluid regularly bathes the eye and then drains through a mesh-like pathway out of the eye. But when the fluid can’t drain properly, pressure inside the eye builds up. Over time, this increased eye pressure may damage the optic nerve.
What are the types of glaucoma?
Chronic (Open Angle) Glaucoma
- Most common type
- Aqueous fluid drains too slowly causing pressure to build up
- More common as you age, but can occur at any age
Acute (Angle Closure) Glaucoma
- Occurs when the drainage system of the eye is closed causing a sudden increase in pressure
- Requires emergency care
- Symptoms may include blurred vision, severe headaches, eye pain, nausea, vomiting or seeing rainbow-like halos around lights
Normal Tension Glaucoma
- Not related to increased eye pressure
- May be caused by reduced blood supply to the optic nerve
- Can cause early central vision loss
Secondary Glaucoma
- Results from another eye condition or disease, such as inflammation, steroid use, diabetes or other retinal conditions, trauma, or tumor
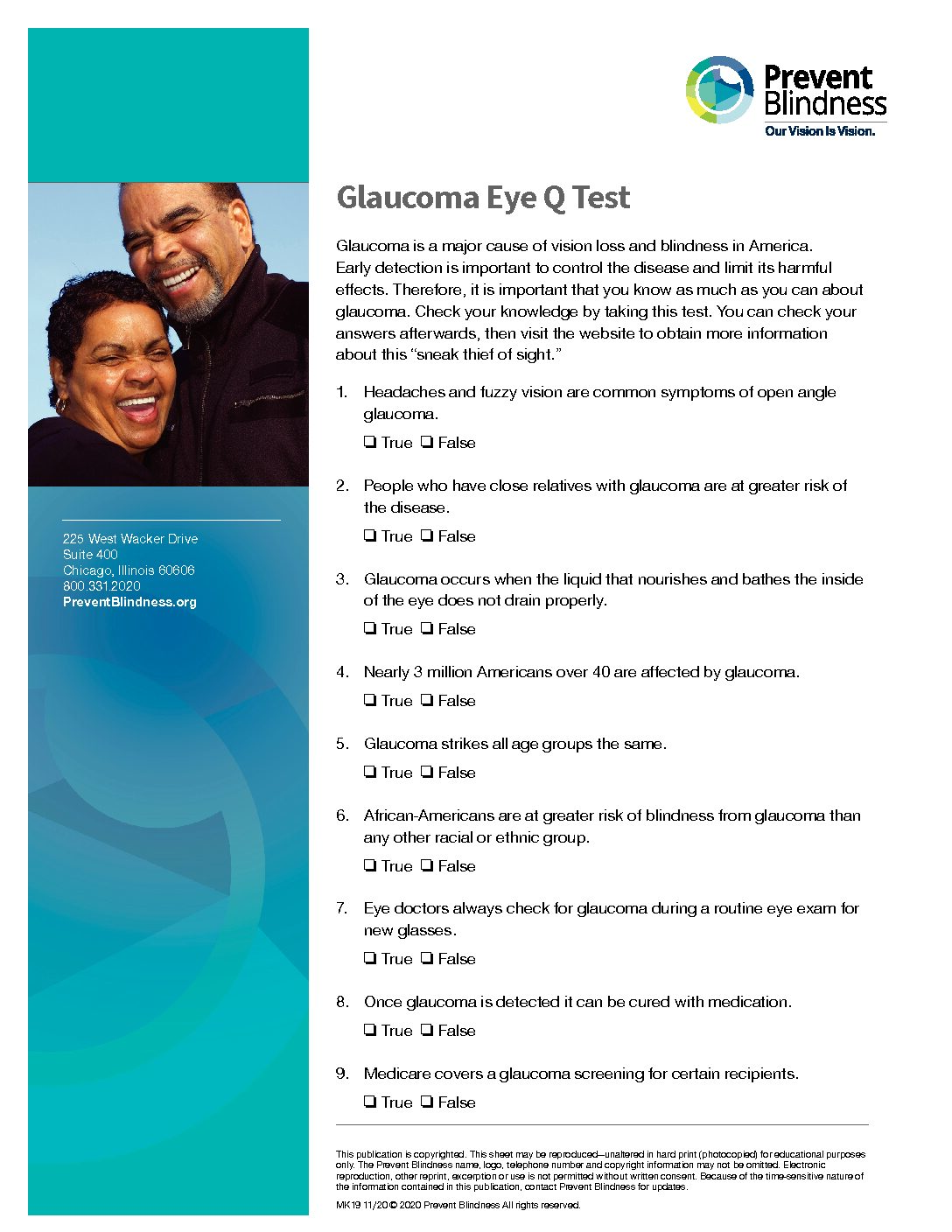
What symptoms might I have with glaucoma?
Glaucoma usually progresses slowly over several years. In most cases, people do not experience any symptoms during the early stages of glaucoma. Usually, glaucoma affects side vision (peripheral vision) first. You may notice that you begin bumping into things on one or both sides of your body, such as furniture, clipping corners, and not initially seeing people or objects and then seeing them after a second look. Later in the disease, glaucoma may cause “tunnel vision” meaning the person can only see straight ahead. That’s why someone with advanced glaucoma can have good straight ahead (central) vision, with very little peripheral vision. However, even central vision can be seriously damaged due to glaucoma.


Simulated loss of peripheral vision from glaucoma
How is glaucoma diagnosed?
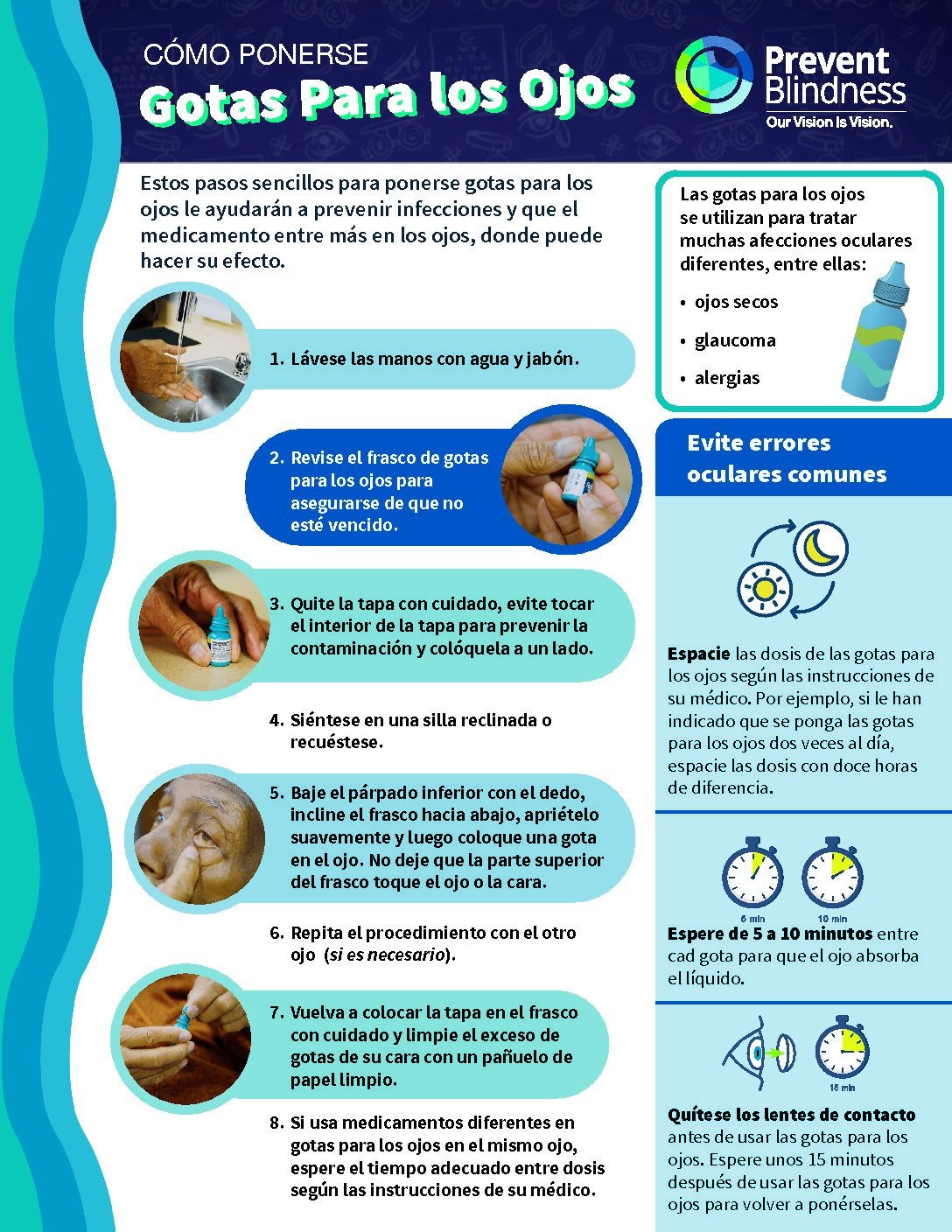
Diagnosis of glaucoma typically starts during an eye examination with an eye doctor (optometrist or ophthalmologist). The eye doctor looks for signs of glaucoma by checking for changes in the appearance of the optic nerve or signs of damage, increased eye pressure (elevated intraocular pressure), and vision loss (visual field loss). The eye doctor may conduct the following tests:
Tonometry: After numbing the eye with medicine drops, an instrument gently presses on the outside of your eye to measure the pressure. This is painless. Pressure can also be measured without eye drops and touching the eye, known as the air puff test.
Gonioscopy: After numbing the eye, the doctor gently places a special lens on the surface to examine the area in the front of the eye that drains fluid. Gonioscopy allows a more accurate diagnosis of the type of glaucoma.
Ophthalmoscopy: The doctor will place a few drops in your eye to open or dilate the pupil. This allows the doctor to examine the optic nerve and retina in the back of the eye.
Perimetry: This test evaluates your visual field (side and central vision) to see if any areas are affected. It usually involves staring straight ahead at a target and trying to see lights that appear around the sides of your view. This is generally done with a computerized system.
Optic Nerve and Retinal Imaging: Digital pictures are taken to show the appearance of the optic nerve inside your eye. An OCT will show the thickness of various layers to see if they have become thinner. This may also involve dilating your eye.
What is the treatment for glaucoma?
Glaucoma can usually be treated and controlled using medicine(s), laser surgery, surgery, or a combination of these treatments. Medicines (eye drops) or laser trabeculoplasty are typically the first step in treatment, but in recent years, new and minimally invasive glaucoma surgical therapies have become available. These therapies, unlike more invasive glaucoma procedures, can be appropriate treatments for mild to moderate disease, alongside medical and/or laser treatments. They can be done on their own or combined with cataract surgery. You and your doctor will work together to decide which treatment plan is best for you.
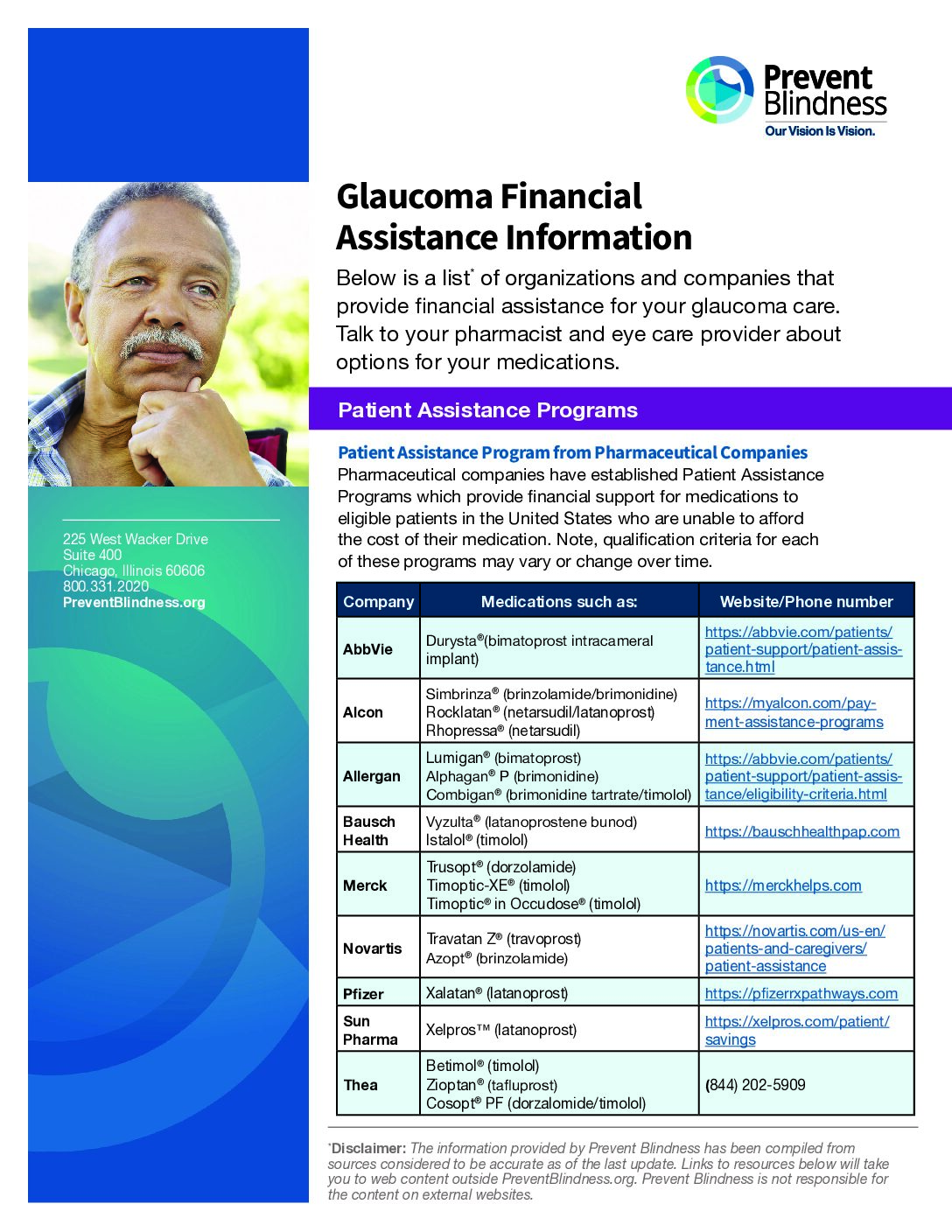
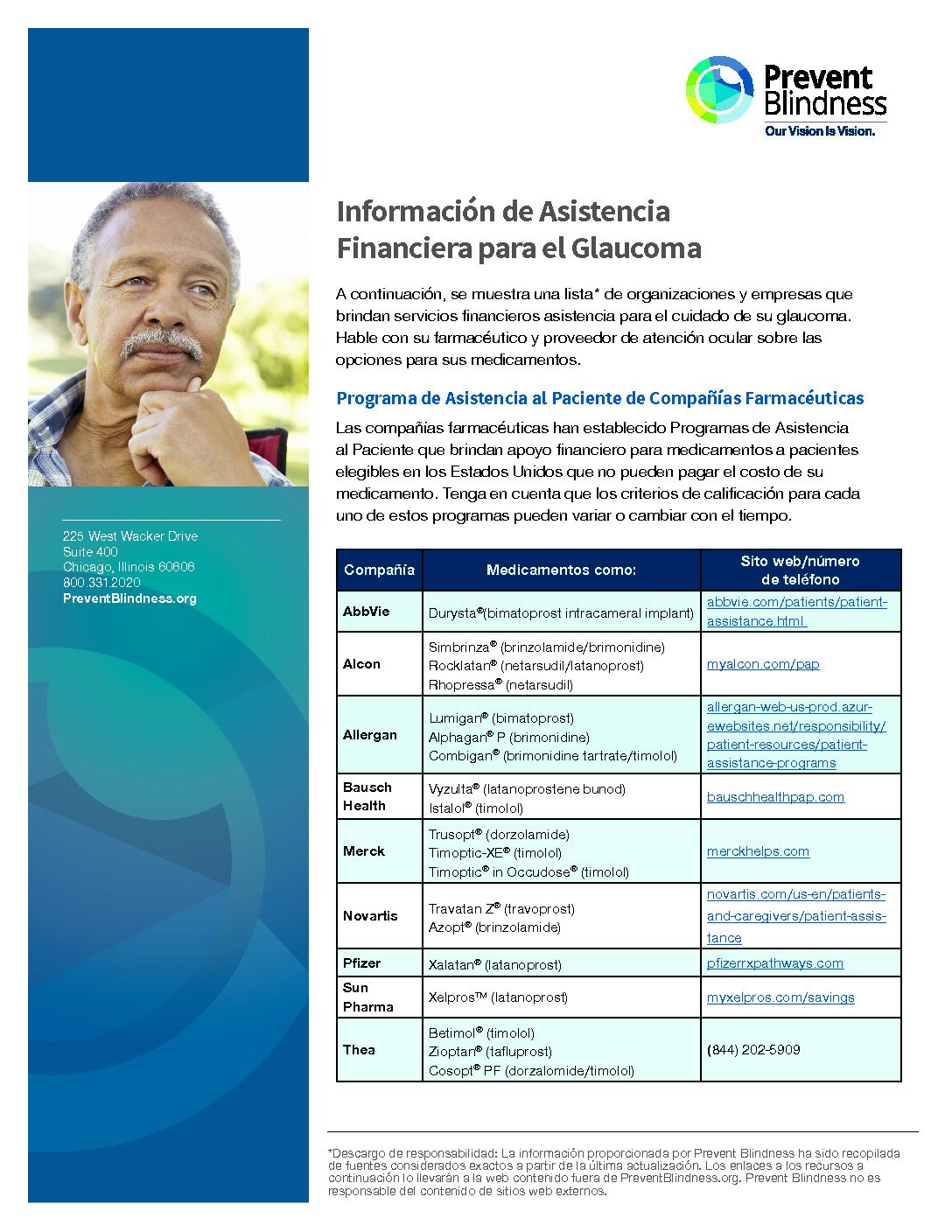
Medicines
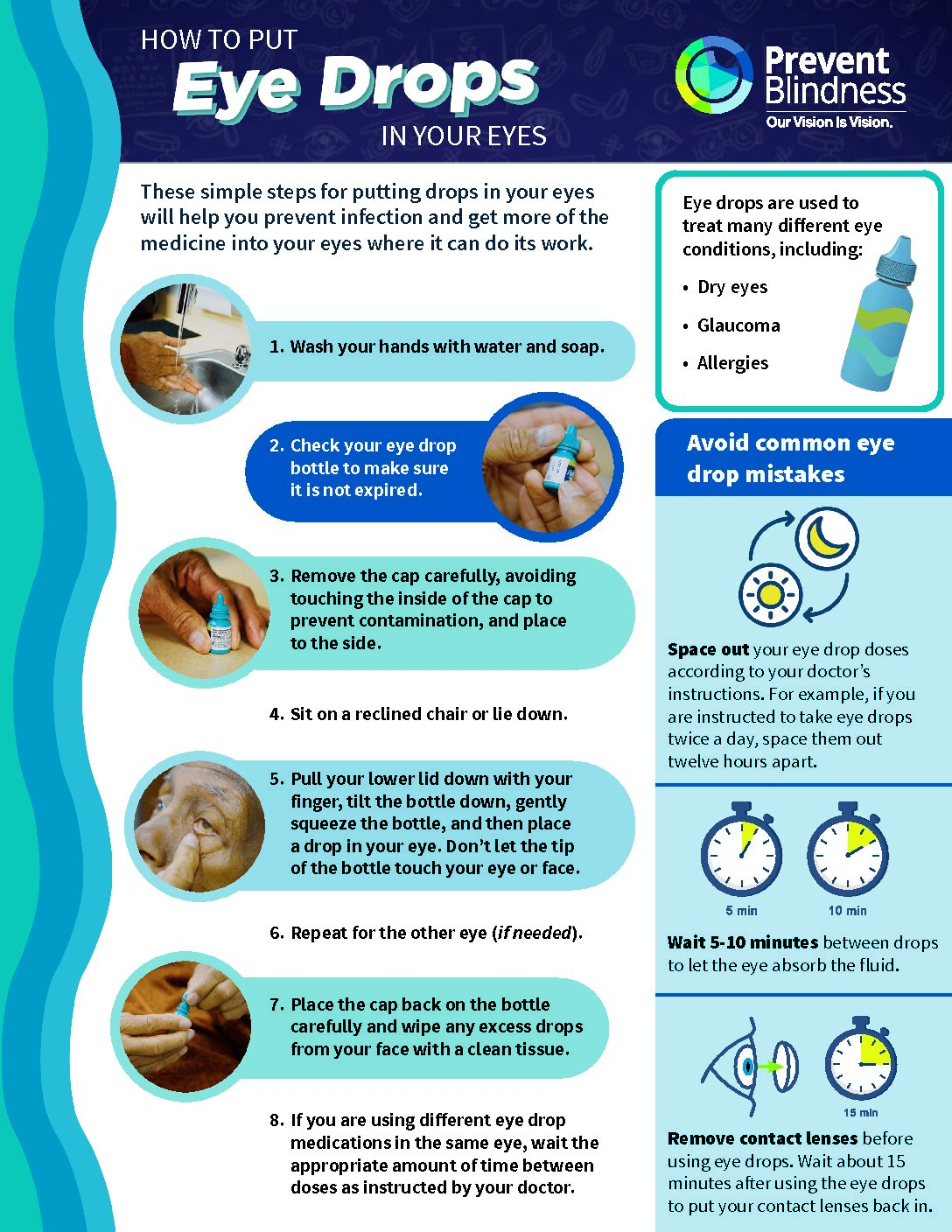
Glaucoma medicines reduce eye pressure by lowering the amount of aqueous fluid produced and/or improving fluid drainage in the eye. These medications are usually in the form of eye drops but also come as pills or ointment. Pills are not used for long term treatment. There are also relatively new, FDA approved, treatment options for an implant into the eye that can release glaucoma medication continuously into the eye. Often, people with glaucoma must take medicine for life to control their eye pressure and limit vision loss. In some patients with early or mild glaucoma a laser treatment can control the pressure for many years.
All glaucoma medicines may cause side effects, some of which can be uncomfortable. A few side effects can be quite serious, but those side effects are not common.
Some people with glaucoma may feel that because their vision seems normal or does not seem to be getting worse, they don’t really need to use medication or have laser treatment. The truth is, skipping doses of your medicine may put your vision in danger – causing additional vision loss. Be sure to tell your doctor if you’ve missed any doses.
Laser surgery
Lasers may be very useful for treating glaucoma because they avoid cutting and are very safe.
Laser surgery is usually successful, but there are some risks. These include a temporary, generally short-term increase in eye pressure and temporary inflammation of the eye.
People usually don’t feel any pain with these procedures, although some report a slight stinging. Most patients take it easy the day of their treatment but go back to their normal routine the following day.
Many people need to keep taking medicines even after laser surgery.
Glaucoma surgery
There are several surgical options for treating glaucoma:
- Filtering surgery: Creates a new path through the eye’s tissues to let fluid drain from the eye
- Drainage implant surgery: A tiny tube is inserted through the sclera into the front part of the eye to drain fluid away
- Minimally invasive glaucoma surgeries: Places a stent or opens the drain of the eye to help fluid flow through the natural drain
- Laser cyclophotocoagulation: Removes tiny areas of the ciliary body that make aqueous fluid to decrease the amount of fluid made. This helps lower the pressure in the eye
How does glaucoma affect mental health?
Glaucoma can cause loss of vision. For some, loss of vision can lead to feelings of depression, anxiety, and loss of independence. Some individuals may notice a change in their desire to socialize with others, or increased frustration with the additional time it may take to accomplish tasks of daily living. Not everyone who has vision loss will experience mental health symptoms, but if you do, there is help available.
To help support your mental health as you live with glaucoma:
Talk to your primary care doctor, mental health professional, or eye doctor: Talk to your doctor about any changes in your emotional well-being. Ask your eye doctor questions about how glaucoma will affect your daily life and work. Seek assistance on how to cope with the changes in your life due to glaucoma.
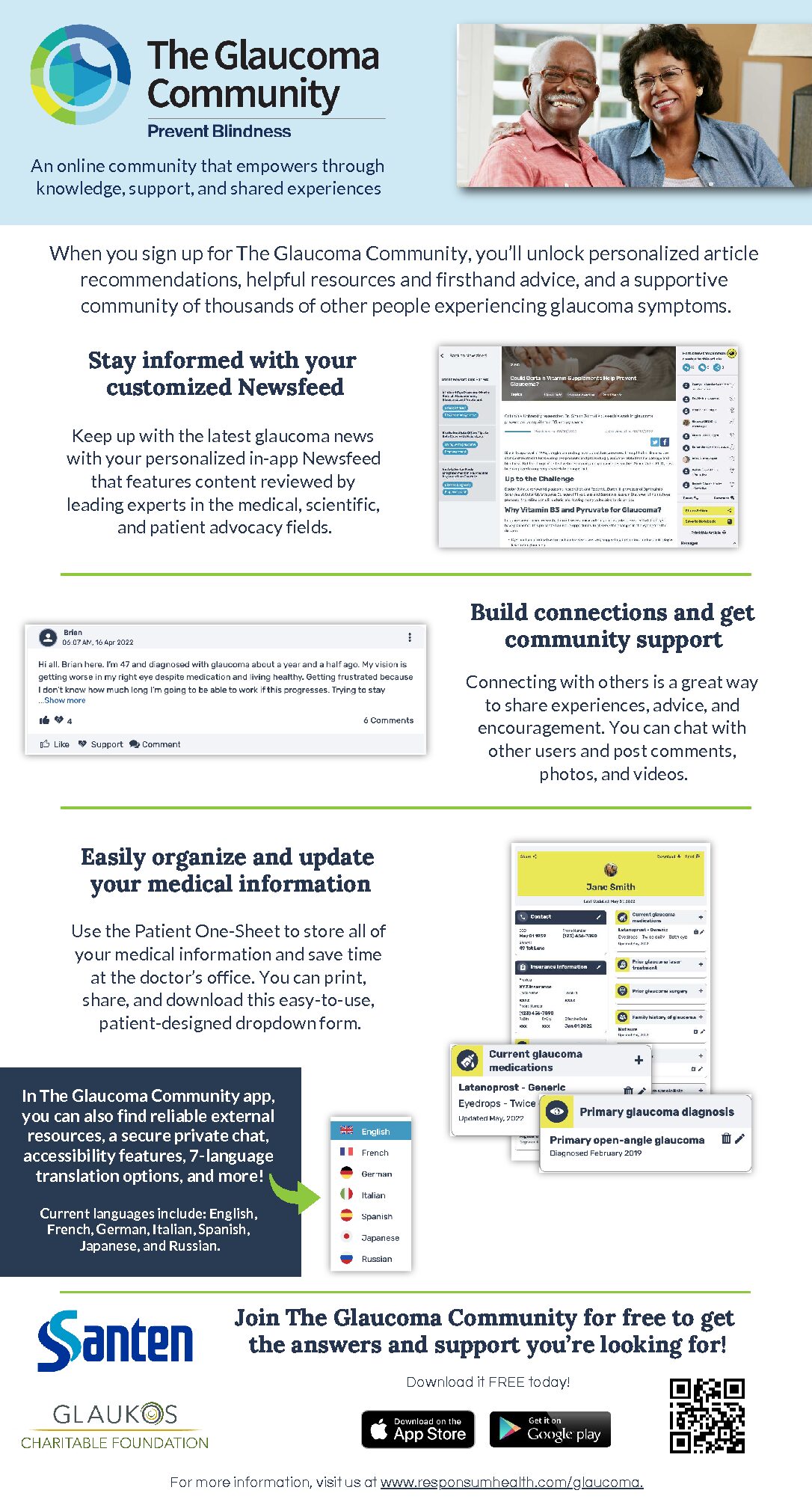
Seek support: Look for support groups of others who have glaucoma, through The Glaucoma Community, in person, and social media groups. These groups can help you learn about your condition, share your experience, and find support.
Connect with others and the things that bring you joy: Stay connected with friends and family to keep you from feeling isolated. Over time, you can find new ways to do the things you love or discover new hobbies that bring you happiness.
Exercise: Physical activity can improve symptoms of depression or anxiety and help you feel better. Certain types of exercise are not recommended for people with glaucoma, so talk to your health care professional to determine what exercise routine may work best for you.
Seek vision rehabilitation: Ask your eye doctor to recommend a low vision specialist. The specialist can help to maximize the use of the vision you have by providing training for adaptive equipment; mobility education, and safer ways to perform household activities. Occupational therapists can evaluate your home to make sure it is safe for you.